Personality Changes and Dementia
A Few Early Signs of Alzheimer's
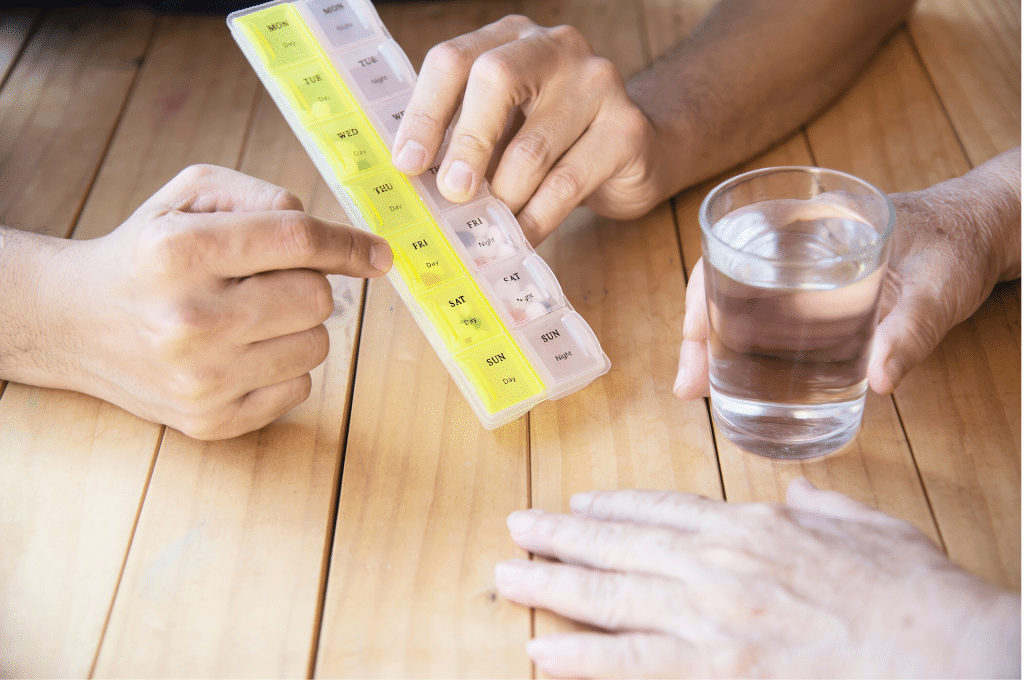
- Lapse in memory that disrupts daily life
- Challenges solving problems
- Trouble making plans
- Mixing up time and places
- Problems using words in speaking and writing
- Misplacing things and then not being able to retrace steps to locate
- Overall decrease in judgement - trouble making decisions
- Withdrawal from social activities
- Change in mood or personality
What would a change in personality mean?
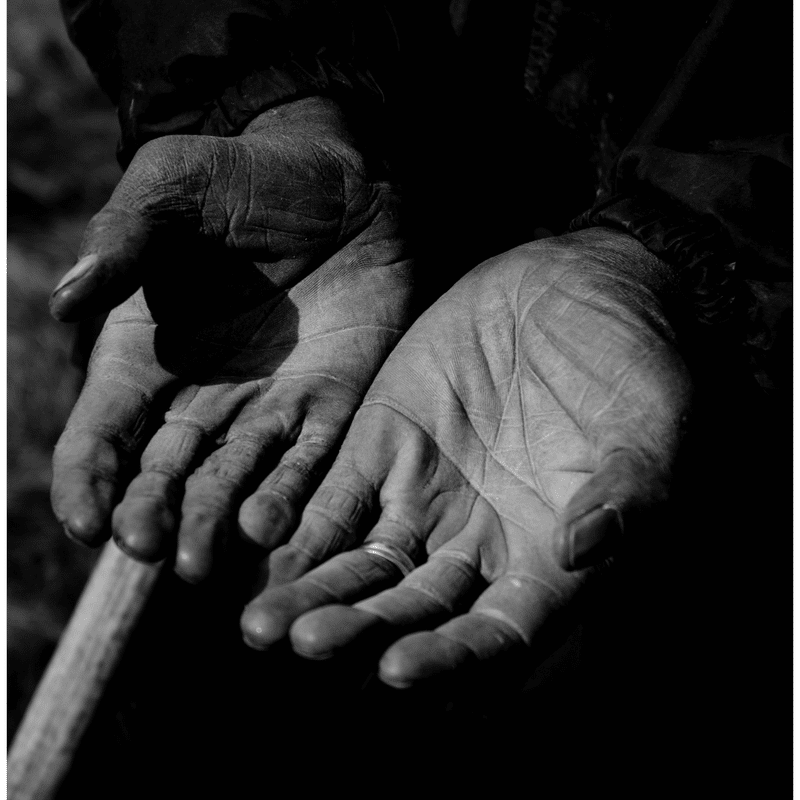
Personality is something that we rather take for granted. It is true that certain aspects of it are inborn, but there are other aspects of one's personality or at least of the persona that they portray, that are learned and practiced over time. We come to depend upon how well we know a person because their personality remains consistent over time. We know, for instance, whether they are generally polite or cranky. We know if they are honest or tend to lie. We know if they tend to be soft-spoken or loud. All of these things help us to feel as though we are on solid ground when describing who a person is. But once dementia or Alzheimer's enters the picture, the ground can begin to shift right under our feet.
Because different types of dementia affect different parts of the brain, the disease may affect personality and behaviors in different ways. If a person has dementia that affects the frontal areas of the brain, their personalities may seem to shift more drastically. It's an important thing to ask about at onset so that you can begin to prepare yourself mentally for how you will deal with the changes you may encounter in the coming months and years. Generally speaking, most individuals with dementia do not completely change their personality. For instance, a person who was nice and calm would not become violent, unless there were other issues such as hallucinations or drug interaction problems going on, but it can occur. Most often the changes that occur are an amplification of their former personality. A soft-spoken person may become even quieter. An angry person may become very overbearing and upset easily.
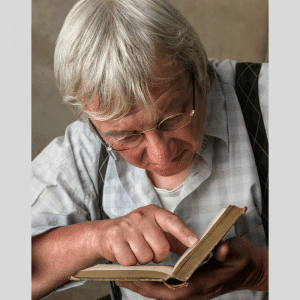
As the disease progresses into advanced stages, several of a person's learned behaviors begin to fade. If they were a voracious reader, they may lose the ability to read. If they wrote often, they will most likely lose that ability. If these were important things to them, and particularly if they were activities that you shared with them, it can seem as though you do not know who they are anymore. We often associate people and our relationships through hobbies and interests. This can also, understandingly, cause a great deal of frustration on their part. They are losing things that they consider to be important parts of themselves. During their lucid moments, if they recognize any of this, it will be frustrating and disappointing to them.
While there is not much that one can do to prevent this from occurring in the advanced stages of the disease, we can begin to prepare ourselves by knowing the likelihood that these changes may occur. We can also take time while we have it, to enjoy their true personality that we've grown to love over time. Take every opportunity to spend time with them and support them through this scary time, assuring them that whatever happens, you'll still remember their true nature. And as you speak of them to others, you'll emphasize who they are rather than the disease to others. This will do more to maintain their dignity than anything else you can do. Their life and personality is a gift to us while our love and care is our gift to them.